(NEW YORK) — Weekly COVID hospitalizations have been ticking up over the past 11 weeks, rising to 20,538 for the week ending Sept. 9, the highest figures seen since March of this year.
Although the majority of U.S. counties are reporting low hospital admissions levels, a growing number are seeing moderate and even high levels, according to data from the Centers for Disease Control and Prevention.
Despite the uptick, doctors and hospital administrators across the country said the number of patients they’ve seen this summer has been lower than previous years and the lessons they’ve learned over the course of the pandemic has helped them cope with increasing hospitalization rates.
In Sacramento County, California, hospital admissions have reached medium levels with about 10.1 admissions per 100,000.
Michael Korpiel, president of the Sacramento market for Dignity Health, a nonprofit that operates hospitals in three states, said there have been fewer than 20 people testing positive for COVID at any time in the six hospitals.
“The last three years have been a great learning experience for our system and our hospital, but I think for the Sacramento region, we are better prepared today than we have been in the past,” he told ABC News. “We have shored up all of our supply lines, so that we make sure that we have enough equipment and supplies in place if we begin to see a spike in the number of COVID patients.”
Similarly, Dr. Rami Zebian, chief medical officer for the Medical University of South Carolina Health Pee Dee Division — which encompasses three hospitals — told ABC News there has not been a huge surge in patients over the summer, but lessons learned have helped the division be prepared.
One example he gave was increasing the number of devices for non-invasive ventilation and knowing when to use ventilation on a patient.
“We have that equipment that can be used for both,” he said. “We learned that we don’t have to put people on the ventilator early on in their disease. If we can delay that, until they really need it, we don’t have to do it.”
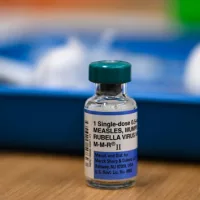
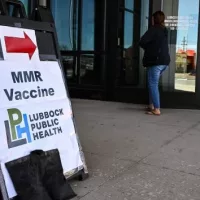
Hospital staff are also kept safe by having enough personal protective equipment when dealing with patients. They’re also encouraged to get the annual flu shot and the updated COVID vaccine that targets circulating variants.
None of the hospitals or health systems that ABC News spoke to said they have universal masking in place, but there are discussions about what the threshold would be to reinstate a mandate or if they would follow county health department guidelines.
As the U.S. moves into the colder weather months — the traditional respiratory virus season — hospitals also need to prepare for a possible “tripledemic,” a mix of COVID, flu and RSV that could overwhelm health systems.
Dr. David Hirschwerk, an infectious disease specialist and the medical director at Northshore University Hospital in New York, said his hospital is in “a constant state of readiness for COVID” as well other viruses.
Nassau County, where NU Hospital is based, is currently in the medium admission category with 10.4 hospital admissions per 100,000, CDC data shows. Hirschwerk said the hospital has not been overwhelmed so far and protocols are in place to prevent it from becoming overwhelmed later in the year.
“Each year as we get into this time of year and as we move deeper into the fall and winter will be impacted by increase in respiratory viruses not only with COVID but also with influenza and other respiratory viruses like RSV,” he told ABC News. “With that we have the tools to do testing, we have the space in our hospital, and we always manage and try to keep our environment safe by testing patients when it’s indicated by screening visitors.”
“It would be great if we don’t see all three viruses simultaneously. But we know that we’re going to see all three at some point and we’ll be prepared regardless of how much there is and what the timing of it is,” Hirschwerk added.
Copyright © 2023, ABC Audio. All rights reserved.