(NEW YORK) — A new study on pregnant people and COVID-19 vaccines is adding to the growing body of evidence showing the vaccine is safe during pregnancy.
Researchers at Northwestern University studying people who had been fully vaccinated during pregnancy, found the vaccine had no impact on pregnancy and no impact on fertility, menstruation and puberty.
The study, published May 11 in the journal Obstetrics & Gynecology, is believed to be the first to examine the impact of the COVID-19 vaccines on the placenta, according to the university.
“At this point, as we’re collecting data, the news is reassuring that this vaccine is safe, both based on its biology and what we’re actually seeing in the real world,” said Dr. Jennifer Ashton, ABC News chief medical correspondent and a board-certified OBGYN.
Here is what pregnant and breastfeeding people may want to know about the COVID-19 vaccines to help them make informed decisions.
1. When can pregnant people get a COVID-19 vaccine?
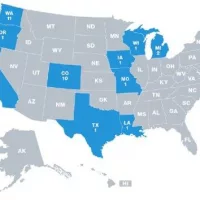
Everyone 12 years of age and older, including pregnant people, is now eligible to get a COVID-19 vaccination, according to the U.S. Centers for Disease Control and Prevention (CDC).
Pregnant people can get the COVID-19 vaccine at any point in their pregnancy, and the vaccine does not need to be spaced from other vaccines, like the flu shot or Tdap booster.
2. What is the science behind the COVID-19 vaccine?
Both the Pfizer and Moderna vaccines use mRNA technology, which does not enter the nucleus of the cells and doesn’t alter the human DNA. Instead, it sends a genetic instruction manual that prompts cells to create proteins that look like the virus a way for the body to learn and develop defenses against future infection.
They are the first mRNA vaccines, which are theoretically safe during pregnancy, because they do not contain a live virus.
The Johnson & Johnson vaccine uses an inactivated adenovirus vector, Ad26, that cannot replicate. The Ad26 vector carries a piece of DNA with instructions to make the SARS-CoV-2 spike protein that triggers an immune response.
This same type of vaccine has been authorized for Ebola, and has been studied extensively for other illnesses — and for how it affects women who are pregnant or breastfeeding.
The CDC has concluded that pregnant people can receive the Johnson & Johnson one-shot vaccine after reviewing more than 200 pages of data provided by the company and the U.S. Food and Drug Administration (FDA).
Vaccine experts interviewed by ABC News said although pregnant women are advised against getting live-attenuated virus vaccines, such as the one for measles, mumps and rubella, because they can pose a theoretical risk of infection to the fetus, the Johnson & Johnson vaccine doesn’t contain live virus and should be safe.
3. Are there studies on pregnant women and the COVID-19 vaccine?
In addition to the most recent Northwestern University study, a study published in the American Journal of Obstetrics & Gynecology in March found the Pfizer and Moderna vaccines are safe and effective in pregnant and lactating people and those people are able to pass protective antibodies to their newborns.
Researchers studied a group of 131 reproductive-age women who received the Pfizer or Moderna vaccine, including 84 pregnant, 31 lactating and 16 non-pregnant women and found antibody levels were similar in all three groups. No significant difference in vaccine side effects were found between pregnant and non-pregnant study participants.
The study had some limitations. It was small and participants were primarily white health care workers from a single city. On the other hand, it’s the largest study of a group that was left out of initial vaccine trials.
4. What are health groups saying about the COVID-19 vaccine?
The World Health Organization (WHO) recently updated its guidance to say pregnant people at high risk of exposure to COVID-19 and those at risk of severe disease should be vaccinated.
“While pregnancy puts women at higher risk of severe COVID-19, very little data are available to assess vaccine safety in pregnancy,” WHO said in a statement. “Nevertheless, based on what we know about this kind of vaccine, we don’t have any specific reason to believe there will be specific risks that would outweigh the benefits of vaccination for pregnant women. For this reason, those pregnant women at high risk of exposure to SARS-CoV-2 (e.g. health workers) or who have comorbidities which add to their risk of severe disease, may be vaccinated in consultation with their health care provider.”
The CDC says people who are pregnant and breastfeeding “may choose to be vaccinated” and should talk with their health care provider, noting that breastfeeding is an important consideration but “is rarely a safety concern with vaccines.”
The American College of Obstetricians and Gynecologists (ACOG), a professional membership organization for OB-GYNs, says both pregnant and breastfeeding people should have access to the vaccine when they are eligible for it, according the criteria of the CDC’s Advisory Committee on Immunization Practices (ACIP).
Likewise, the Society for Maternal-Fetal Medicine (SMFM) recommends pregnant people have access to vaccines and says pregnant people should “engage in shared decision-making” about the vaccine with their doctors.
“In general, SMFM strongly recommends that pregnant women have access to COVID-19 vaccines in all phases of future vaccine campaigns, and that she and her health care professional engage in shared decision-making regarding her receipt of the vaccine. … mRNA vaccines, which are likely to be the first vaccines available, do not contain a live virus but rather induce humoral and cellular immune response through the use of viral mRNA,” the society said in its statement. “Health care professionals should also counsel their patients that the theoretical risk of fetal harm from mRNA vaccines is very low.”
5. What will clinical trials be like for pregnant people?
Pfizer’s phase 2/3 trial will enroll approximately 4,000 women within weeks 24-34 of their pregnancy, the company announced in a press release.
Half will get the vaccine, and half will get a placebo.
The study will include healthy, pregnant woman age 18 and older in the U.S., Canada, Argentina, Brazil, Chile, Mozambique, South Africa, the United Kingdom and Spain.
Participants in the vaccine group will receive two doses at 21 days apart — and each woman will be followed for at least 7-10 months in order to continuously assess for safety in both participants and their infants.
Infants will also be assessed, up until 6 months of age, for transfer of protective antibodies from their vaccinated mother.
Women enrolled in the trial will be made aware of their vaccine status shortly after giving birth to allow those women who originally received placebo to be vaccinated while staying in the study.
6. Why weren’t pregnant people included in early clinical trials?
Not recruiting parents-to-be in clinical trials and medical research is nothing new, according to Dr. Ruth Faden, the founder of the Johns Hopkins Berman Institute of Bioethics and a bioethicist who studies the ethics of pregnancy and vaccines.
“For a very long time, pregnant women were not included in biomedical research evaluation efforts or clinical trials, both for concerns about fetal development and what would be the implications of giving a pregnant women an experimental drug or vaccine and also for legal liability worries from manufacturers and pharmaceutical companies,” Faden told “GMA” last month. “There’s a huge gap between what we know about the safety and effectiveness of a new drug or a new vaccine for the rest of the population and what we know about it specific to pregnancy.”
In the case of the COVID-19 vaccines, health experts have only one of the three sources of evidence that are used to evaluate safety and efficacy during pregnancy: the data on non-pregnant people who were enrolled in the clinical trials, according to Faden.
From that, Faden said, health experts can try to glean what side effects may happen to people who are pregnant, but it is not an exact science.
However, it’s considered typical — and many argue ethically appropriate — to study an unknown substance first in healthy adults and then progressively in broader and broader populations. Pregnant people and children are often tested later down the line because of concerns about potential long-term harm.
Some of the volunteers in prior COVID-19 vaccine trials that didn’t include pregnant women directly may still become pregnant during the trial. This will also give researchers some insights about the vaccine’s safety among this group.
Former commissioner of the U.S. Food and Drug Administration (FDA), Dr. Stephen Hahn, told ABC News in December that the agency planned to look at that data.
“In the clinical trials, we did not require a pregnancy test for entry into the clinical trials, which means that when we look at the data, there are likely going to be women of childbearing age who have gotten pregnant,” then-commissioner Hahn told ABC News chief medical correspondent Dr. Jennifer Ashton in an interview on ABC News’ Instagram Live. “So we are likely to be able to see data. I can’t prejudge those data, but it’s one of the things we’ll have to look at.”
“Will that be enough data for us to have confidence and say pregnant women should be vaccinated? I think that’s something that we’ll have to take a look at,” he added.
7. What risk factors should pregnant people consider?
At this time, the CDC recommends that pregnant women be prioritized for vaccinations and encourages them to speak to their doctors about the risks and benefits of a vaccination.
The question of whether an expecting parent should receive a COVID-19 vaccine will eventually come down to a number of factors, including everything from the trimester, risk factors for COVID-19, ability to remain socially distanced in their lifestyle and occupation, guidance from federal and state officials and recommendations from a person’s own physicians, experts say.
Similar to the flu vaccine, which was not tested on pregnant people in clinical trials, health experts will need to rely on continuously incoming data to make decisions around how safe the COVID-19 vaccines are during pregnancy.
Officials are doing the same for the general population, considering the speed at which the COVID-19 vaccines were developed, according to Faden, who noted that people who are pregnant should not be “unnecessarily alarmed.”
The COVID-19 vaccines can be taken during any trimester. Since other vaccines are recommended during pregnancy, the CDC currently recommends spacing out vaccine appointments a few weeks apart, if possible.
8. Is COVID-19 more dangerous for pregnant people?
Even now, more than one year into the coronavirus pandemic in the U.S., some questions remain about how pregnant people are impacted by COVID-19.
The CDC has shared data showing that pregnant people infected with COVID-19 are at an increased risk for “intensive care unit admission, invasive ventilation, extracorporeal membrane oxygenation, and death,” compared to nonpregnant people.
Health experts say that with or without the vaccine, pregnant people need to continue to remain on high alert when it comes to COVID-19 by following safety protocols, including face mask wearing, social distancing and hand washing.
Copyright © 2021, ABC Audio. All rights reserved.